Everyone has heard of diphtheria, but this familiar infection caused by a Corynebacterium strain isn’t the only illness laboratories should be concerned about. Sterile manufacturing facilities should also be on the lookout for non-diphtherial Corynebacterium. These strains, commonly found in normal skin flora, can be harmful to immunocompromised patients using medical or prosthetic devices.
Colony Appearance: Corynebacterium spp. form small, circular, convex, white to gray colonies on non-selective media such as Sheep Blood Agar and Tryptic Soy Agar.
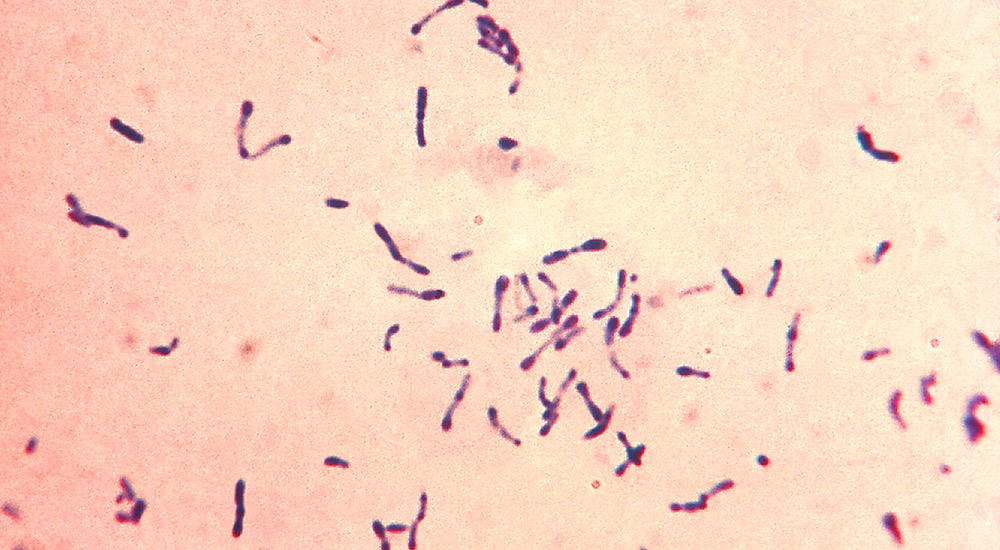
Microscopic Characteristics: Corynebacterium spp. are short, Gram-positive rods (bacilli). The club-shaped rods inspired the name coryneform, which means “club-shaped.”1
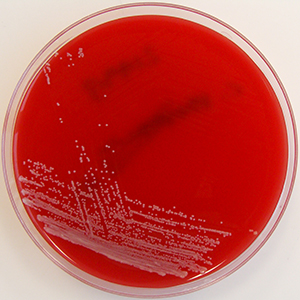
Corynebacterium striatum on Horse Blood Agar (Source: Wikimedia Commons)
Conditions for Growth: Corynebacterium spp. are aerobic, grow best at 30°C – 35°C, and are slow growing. Most Corynebacterium are not lipophilic, and can be either fermentative or non-fermentative. They are Gram-positive, non-motile, and non-spore forming.
Habitat: Corynebacterium spp. are common in nature as well as the normal skin flora and mucosa of humans and animals.
Pathogenicity: Diphtheria is the most well-known human infection caused by a Corynebacterium strain. Corynebacterium diphtheriae obtains the ability to produce diphtheria toxin after interacting with a bacteriophage. Infected patients can experience respiratory problems including difficulty breathing and swallowing due to a thick gray coating that can build up in the throat and nose.
Other species of Corynebacterium can also be pathogenic, particularly in immunocompromised individuals. These other species of Corynebacterium are collectively referred to as non-diphtherial Corynebacterium. 2 One of these strains, Corynebacterium striatum, is developing as a multidrug-resistant bacterium by showing resistance to penicillin, tetracycline, clindamycin, erythromycin, and ciprofloxacin.3
Environmental Risk: Because Corynebacterium is part of the skin microbiota, it can be cause for concern in sterile manufacturing. The potential pathogen likely lives on technicians’ skin. The most probable setting for non-diphtherial Corynebacterium infections is medical devices or prosthetic devices.4
Knowing that Corynebacterium is commonly recovered in cleanrooms can help determine appropriate disinfection regimens, air handling systems, and cleanroom control. Laboratories can also:
- Educate laboratory personnel on how to identify Corynebacterium by morphology or using an identification system that can detect the organism
- Collect environmental monitoring samples to detect Corynebacterium in the manufacturing facility and continue using the isolate for routine QC to ensure their processes can detect it
Taxonomy:
| Kingdom: | Bacteria | Order: | Actinomycetales |
| Phylum: | Actinobacteria | Family: | Corynebacteriaceae |
| Genus: | Corynebacterium |
Looking for Corynebacterium QC strains? Microbiologics offers many distinct species of Corynebacterium in easy-to-use formats.
If you’ve isolated Corynebacterium in your laboratory, we can simplify your next steps. Send us your isolate for custom preservation and you will receive a QC testing kit designed for your lab with your isolate. Visit our website to learn more.
References:
1 Corynebacterium Wikipedia https://en.wikipedia.org/wiki/Corynebacterium
2 Corynebacterium Infections (2017) https://emedicine.medscape.com/article/215100-overview
3 MultiDrug-Resistant Corynebacterium striatum Associated with Increased Use of Parenteral Antimicrobial Drugs (2016) https://wwwnc.cdc.gov/eid/syn/en/article/22/11/16-0141.htm
4 Corynebacterium https://www.sciencedirect.com/topics/medicine-and-dentistry/corynebacterium




If a person has a multidrug resistant strain of Corynebacterium living on their skin, can if cause disease on that person if say they get a laceration or puncture on the skin?