In a world where antibiotic resistant organisms are on the rise, including multi-drug resistant strains of N. gonorrhoeae, it’s more important than ever for clinicians and healthcare providers to provide proper and timely treatment for infections. Complex interactions exist between the human microbiota and overall health, and the vaginal ecosystem is no exception.
Vaginitis is a poorly understood condition despite its prevalence within the population, and as such it often is not treated correctly. Untreated or improperly treated vaginal infections such as those discussed in this post can result in deleterious conditions including an increased risk of contracting additional sexually transmitted infections (STIs), pelvic inflammatory disease, and pregnancy complications.
About Vaginitis
Vaginitis is a condition which encompasses several disease presentations. An overabundance of pathogenic organism species, typically anaerobic bacteria or yeast, is thought to be one cause, and another confirmed cause is the proliferation of the parasite Trichomonas vaginalis. Healthy vaginal flora is commonly comprised of different species of Lactobacillus which produce lactic acid. This metabolite directly influences the vaginal pH which is normally acidic in healthy individuals and helps to maintain the levels of pathogenic bacteria found there in low concentrations.
These pathogenic organisms include but are not limited to:
- Gardnerella vaginalis
- Candida species (particularly albicans, but also includes other pathogenic species of Candida including C. krusei, C. dubliniensis, C. glabrata, C. parapsilosis, and C. tropicalis)
- Megasphaera species
- Atopobium vaginae
Interestingly, organisms implicated in causing vaginitis may be present in people without symptoms as colonizing species or commensals.
The most common types of vaginitis are:
- Bacterial vaginosis
- While the exact cause of bacterial vaginosis is not known, vaginal flora imbalances are thought to be the root cause
- According to the Centers for Disease Control and Prevention (CDC), bacterial vaginosis affects an estimated 21.2 million individuals in the United States alone
- Bacterial vaginosis can be asymptomatic, and infections can return over time even with treatment
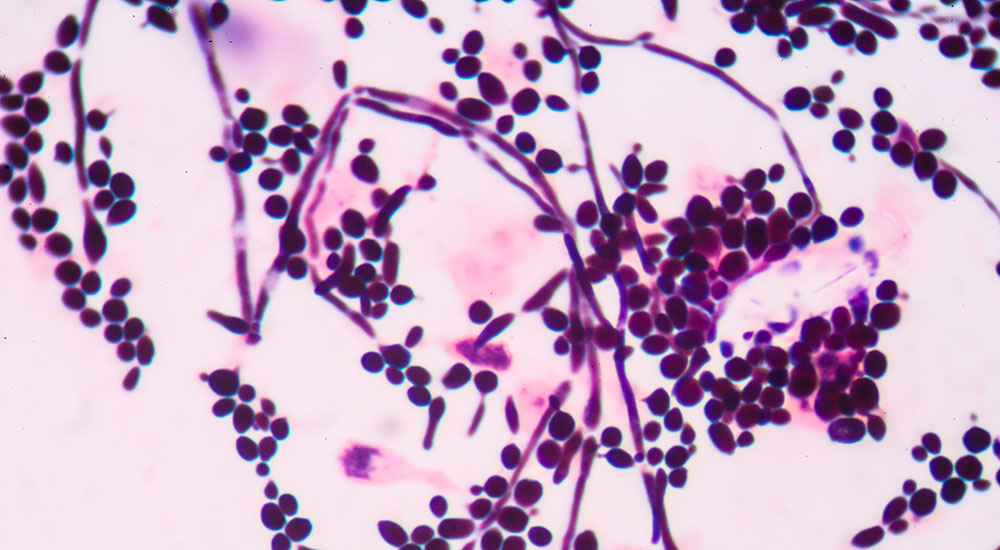
- Vulvovaginal candidiasis
- Known in colloquial terms as a yeast infection
- Caused by a pathogenic proliferation of Candida species, many of which are normal human flora
- Second most common cause of vaginal infections after bacterial vaginosis, though it is not a reportable condition according to the National STD Curriculum
- Trichomoniasis
- Caused by the Trichomonas vaginalis parasite
- One of the most common STIs; an estimated 3.7 million people are infected in the United States according to the CDC
- Although treatments are available, vaginalis can persist in the vaginal environment for years
Importance of Clinical Testing for Vaginitis
The importance of diagnosing the cause of vaginitis manifests in the complexity of the condition and the implications of delayed or improper treatment. As mentioned above, when bacterial vaginosis is present, there is an increased risk of contracting STIs including HIV, gonorrhea, and chlamydia. Since many symptoms of bacterial vaginosis, vulvovaginal candidiasis and trichomoniasis overlap, accurate testing is of the utmost importance. However, first-round clinical testing isn’t organism-specific, and instead is based on shared symptoms. The National STD Curriculum lists tests, encompassing several types of wet mount preparations, potassium hydroxide treatments, Gram stains, and pH testing, as the standard diagnostic procedures for determining a specific vaginitis cause.
Organism-specific Testing Methods
A clinical diagnosis can be obtained using the methods above, but in instances of recurring, particularly onerous, or time-sensitive cases of vaginitis, there are organism-specific tests that can be performed. Pinpointing the exact organism or organisms that produce vaginitis in an individual has many benefits including better treatment tailored to the patient.
Several organism-specific testing methods are available for clinical use:
- Culturing
- Many species implicated in causing vaginitis can be cultured, including Candida species and Trichomonas vaginalis
- Does not differentiate between colonizing species and pathogenic species
- Nucleic acid testing
- Available for Trichomonas vaginalis testing with the Aptima Trichomonas vaginalis Assay manufactured by Hologic®
- Available for Trichomonas vaginalis testing with the Xpert™ Trichomonas vaginalis Assay manufactured by Cepheid®
- Available for Trichomonas, Gardnerella, and Candida in a single system, the BD Affirm™ VPIII microbial identification system
- PCR
- The BD MAX™ Vaginal Panel tests for organisms that cause bacterial vaginosis, vulvovaginal candidiasis, as well as Trichomonas vaginalis
- PCR is a sensitive and specific technology
With timely and accurate testing, vaginitis causes can be determined and treated correctly. Microbiologics offers a variety of quality control products to help your laboratory ensure accurate results when testing for STIs and vaginal infections including:
- Vaginal Control Panel (Inactivated Pellets)
- Vaginal Verification Panel (Inactivated Pellets)
- Trichomonas vaginalis (TV) Control Panel (Inactivated Swab)
- Candida live cultures
- Gardnerella vaginalis live cultures
- Inactivated Trichomonas vaginalis
Visit our website to find the right strains and formats for QC in your lab.
Read Next: Neisseria gonorrhoeae: Combating a Multidrug-Resistance Organism
Resources
https://www.std.uw.edu/go/syndrome-based/vaginal-discharge/core-concept/all
https://www.cdc.gov/std/tg2015/candidiasis.htm
https://www.cdc.gov/std/tg2015/trichomoniasis.htm
https://www.cdc.gov/std/tg2015/bv.htm
https://www.cdc.gov/std/bv/treatment.htm
https://www.mayoclinic.org/diseases-conditions/vaginitis/symptoms-causes/syc-20354707





The Vaginitis defination and diagnosis is eyeopening for me.Here in Kenya we mainly rely on clinical testing due to high cost & unavailbility of organism specific testing methods.I request if you can give me information of affordable organism specific testing methods.
Alex – Unfortunately we can’t provide this information, but our distributor in Kenya may be able to help: Ultralab EA, +254 20 340 998, info@ultralabealtd.co.ke. You can find distributor information on our website as well: http://www.microbiologics.com/locate-a-distributor.