 STEC may not be a household term, but it is of great significance to food and clinical laboratories. In this post, we will describe what laboratories can do to help protect the public from this harmful and increasingly important group of bacteria. The information outlined below relies heavily on content provided by the Centers for Disease Control and Prevention (CDC).
STEC may not be a household term, but it is of great significance to food and clinical laboratories. In this post, we will describe what laboratories can do to help protect the public from this harmful and increasingly important group of bacteria. The information outlined below relies heavily on content provided by the Centers for Disease Control and Prevention (CDC).
What is STEC?
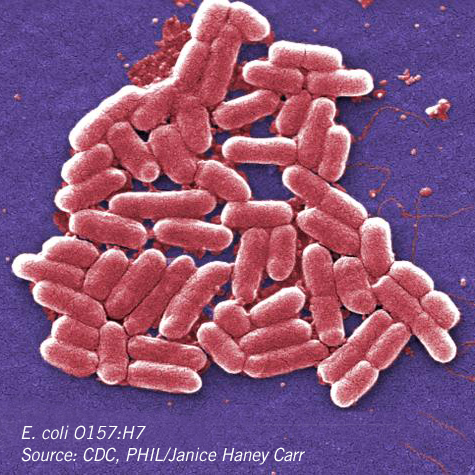
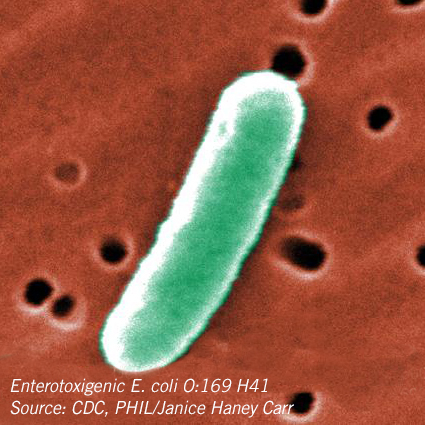
Escherichia coli consists of a diverse group of bacteria, but microbiology laboratories in the United States are most familiar with the pathogenic strain of E. coli O157:H7. All E. coli that produce a Shiga toxin are known as STEC.
STEC serotypes are identified by their somatic (O) and flagellar (H) antigens. Thus, E. coli O157 refers to the O antigen 157, and E.coli O157:H7 identifies the H7 antigen. Non-O157 STEC refers to other pathogenic strains, such as the more commonly referenced serogroups O26, O45, O103, O111, O121, and O145.
Why should you care about STECs?
The CDC estimates there are 265,000 Shiga toxin-producing E. coli infections in the United States each year. Of these infections, 36% are attributed to E. coli O157:H7 and the remaining 64% are cause by non-O157 STECs.
E. coli is transmitted to humans through contaminated food, water, or direct contact with people or animals. E. coli O157:H7 may cause diarrhea, urinary tract infections, pneumonia, or other serious illnesses in humans. Non-O157 STEC also may cause illnesses some of which may be severe such as bloody diarrhea, acute renal failure or death. In order to detect, treat and contain these bacterial enteric infections, accurate and prompt laboratory diagnoses are critical.
 What can labs do?
What can labs do?
According to “Recommendations for Diagnosis of Shiga Toxin-Producing Escherichia coli Infections by Clinical Laboratories” published by The Morbidity and Mortality Weekly Report (MMWR), “All stools submitted for testing from patients with acute community-acquired diarrhea should be cultured for O157 STEC on selective and differential agar.” In addition, these stool samples should be assayed simultaneously for non-O157 STEC with a test that detects the Shiga toxins or the genes encoding these toxins.
What are the procedures for handling specimens?
Laboratories should always consult the manufacturer’s instructions on proper procedures for collecting and handling specimens. According to the MMWR Recommendations, the “ideal specimen for testing is diarrheal stool” collected “as soon as possible after diarrhea begins, while the patient is acutely ill, and before an antibiotic treatment is administered.”
Prompt testing performance will help ensure maximum sensitivity and specificity for STEC detection with available commercial diagnostic assays. The report recommends that STEC testing be performed on growth from broth culture or primary isolation media rather than the less sensitive and less specific direct testing of stool. Enzyme immunoassay (EIA) testing of broth enrichments from stools or of growth from the primary isolation plate is recommended as opposed to direct testing of stools.
 Should labs culture for Non-O157 STEC?
Should labs culture for Non-O157 STEC?
According to the MMWR report, identification of non-O157 STEC usually occurs at the public health laboratory. Yet, it outlined the following procedures for isolating non-O157 STEC as follows:
Shiga toxin positive broth should be streaked to a relatively less selective agar (e.g., MacConkey agar, SMAC, Statens Serum Institut [SSI] enteric medium, or blood agar). Traditional enteric media such as Hektoen agar, xyloselysine-desoxycholate agar, and Salmonella-Shigella agar inhibit many E. coli and are not recommended.
All possible O157 STEC colonies should be tested in O157 latex reagent before isolation of non-O157 STEC is attempted. Well isolated colonies with E. coli-like morphology should be selected on the basis of sorbitol or lactose fermentation characteristics (or other characteristics specific to the medium used); most non-O157 STEC ferment both sorbitol and lactose, although exceptions have been reported (CDC, unpublished data, 2009).
Colonies may be tested for Shiga toxin production by EIA or for stx1 and stx2 genes by PCR. Non-O157 STEC may be tested using commercial O-specific antisera for the most common STEC-associated O antigens (i.e., O26, O45, O103, O111, O121, and O145). Non-O157 STEC isolates should be forwarded to a public health laboratory for confirmation of Shiga toxin production, serogroup determination, and PFGE subtyping.
 What should labs do to support the public health?
What should labs do to support the public health?
Clinical laboratories have a responsibility to assist in protecting the public from STEC. Detection of STEC should be reported by the clinical laboratory to the treating physician as well as to the public health laboratory for confirmation, isolation and subsequent testing of the organism. Appropriate public health authorities should also be notified for further potential outbreak investigation.
CDC recommends that specimens or enrichment broths in which STEC is detected, even if O157 STEC is not recovered, should be forwarded promptly to a state or local public health laboratory. Overall, prompt and early diagnosis of STEC infection is essential for administering proper treatment to patients. As stated in the MMWR Report, “… certain treatments can worsen patient outcomes; for example, antibiotics might increase the risk for HUS (hemolytic uremic syndrome) in patients infected with O157 STEC, and antidiarrheal medications might worsen the illness. Early diagnosis of STEC infection also might prevent unnecessary procedures or treatments…”
Clinical laboratories, by promptly diagnosing and referring STEC isolates, may help to prevent additional infections in food service establishments, ward off secondary transmission in nursing homes and child care facilities, and stop multi-state outbreaks.
Key takeaways
1. Accurate and prompt laboratory diagnoses are critical in detecting, treating and containing bacterial enteric infections.
2. Laboratories should always consult the manufacturer’s instructions on proper testing procedures.
3. STEC testing should be performed on growth from broth culture or primary isolation media rather than direct stool.
4. Detection of STEC should be reported by the clinical laboratory to the treating physician and to the public health laboratory.
5. Specimens or enrichment broths in which STEC is detected should be forwarded promptly to a state or local public health laboratory.
Looking for STEC controls? Visit our website to find the right strain and format for your lab.
Biography
 Robin E. Stombler is President of Auburn Health Strategies, LLC, a strategic and business development company serving health and science clients nationwide. Prior to founding Auburn Health Strategies, Stombler served as the Vice President of Government Affairs for the 140,000 members of the American Society for Clinical Pathology, and directed its Washington Office for over nine years. She previously served as a Senior Washington Associate for the American College of Surgeons. Among her publications, Stombler co-authored Laboratory Preparedness for Bioterrorism: From Phlebotomist to Pathologist; Institute for Quality in Laboratory Medicine: Recognizing Excellence in Practice: Highlights from First Landmark Summit –An Opportunity to Enhance Medical Care; and Food Industry Could Learn from Labs. She has been an invited participant in the Bureau of Health Professions Strategic Planning Forum at the Health Resources and Services Administration as well as a Public Health and Strategic Planning Consultant at the Centers for Disease Control and Prevention.
Robin E. Stombler is President of Auburn Health Strategies, LLC, a strategic and business development company serving health and science clients nationwide. Prior to founding Auburn Health Strategies, Stombler served as the Vice President of Government Affairs for the 140,000 members of the American Society for Clinical Pathology, and directed its Washington Office for over nine years. She previously served as a Senior Washington Associate for the American College of Surgeons. Among her publications, Stombler co-authored Laboratory Preparedness for Bioterrorism: From Phlebotomist to Pathologist; Institute for Quality in Laboratory Medicine: Recognizing Excellence in Practice: Highlights from First Landmark Summit –An Opportunity to Enhance Medical Care; and Food Industry Could Learn from Labs. She has been an invited participant in the Bureau of Health Professions Strategic Planning Forum at the Health Resources and Services Administration as well as a Public Health and Strategic Planning Consultant at the Centers for Disease Control and Prevention.





0 Comments
Trackbacks/Pingbacks