At any given time, one in five people in the US has a sexually transmitted infection (STI), translating to more than 60 million infections per year.1 These infections cost billions in healthcare expenses each year. Even more alarming, over 40% of all new STIs in this country affect those between ages 15 and 24.2 The eight most common STIs tracked by the Center for Disease Control (CDC) are chlamydia, gonorrhea (GC), syphilis, trichomoniasis, human papilloma virus (HPV), herpes simplex virus type-2 (HSV-2), human immunodeficiency virus (HIV) and hepatitis B virus (HBV). If diagnosed early, the four non-viral diseases are easily cured in most cases.1
STIs in the US continued to increase even through the second year of the COVID-19 pandemic, with chlamydia, syphilis, and gonorrhea on the rise. These infections are reported to the CDC through the National Notifiable Diseases Surveillance System, the STD Surveillance Network, and the Gonococcal Isolate Surveillance Project (GISP).3 With an estimated 1.6 million new infections per year, Neisseria gonorrhoeae (N. gonorrhoeae or NG) is the second most reported bacterial STI in the US, according to the CDC. Around half of these infections are resistant to at least one antibiotic.4 From 2017 to 2021, the incidence of Neisseria gonorrhoeae increased by over 40%. (Figure 1).
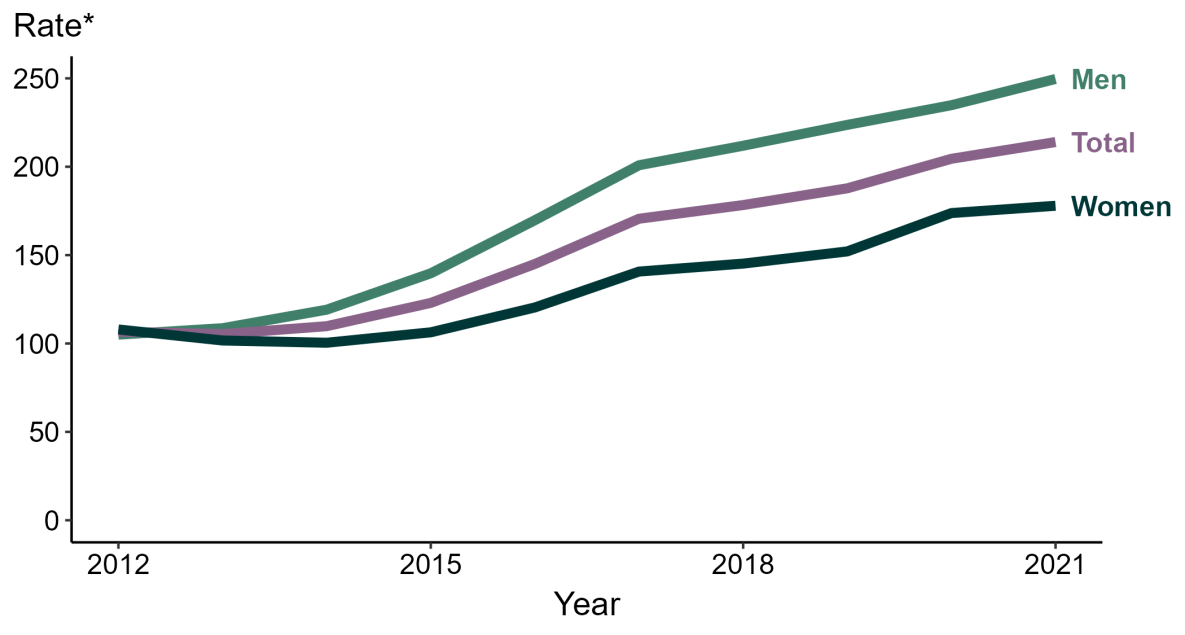
Figure 1: Gonorrhea – Rates of reported cases by sex, United States, 2012 – 2021
*Per 100,000. Source: (5)
Worldwide, the numbers are even more troubling. According to estimates from the World Health Organization (WHO), 2012 saw an estimated 78M new cases among people ages 15 – 49 around the world, with a global incidence rate of 19 per 1,000 women and 24 per 1,000 men. Western Pacific and African regions had the most infections observed.6 There are mainly five reasons for the increases in gonococcal infections and resistance:
- Unrestricted access to antimicrobials
- Inappropriate selection and overuse of antibiotics
- Suboptimal quality of antibiotics
- Inherent genetic mutations within the organism which have contributed to the development of a pattern of resistance in gonorrhoeae
- Extra genital infections – anorectal and pharyngeal – particularly affecting key populations such as men who have sex with men. These extra genital infections may also contribute to the development of resistant strains through the interaction and exchange of genetic material with other co-infections in these anatomical sites6
The Disease
Gonorrhea is a common sexually transmitted disease that can cause infections of the genitals, rectum, and throat. It can be treated and cured, but this organism readily attains resistance to antibiotics.4 It is one of the more troubling STIs, because many people that are infected do not have symptoms and thus can spread it unknowingly.7 Gonorrhea can pose greater risks for women. If untreated, gonorrhea can cause serious and permanent reproductive problems such as ectopic pregnancy; maternal death; first trimester miscarriage; a five-fold increase of HIV transmission; infertility; and severe neonatal eye infections that may lead to blindness. Untreated infections in both men and women can also result in cardiovascular and neurological issues.6
Because of the difficulties in reaching the potentially infected sexual partners of patients being treated for gonorrhea, clinicians can offer Expedited Partner Therapy (EPT), whereby prescriptions or medications are provided to the patients for their partners, forgoing physical exams.8 The goal is to expand therapy as broadly as possible to prevent the further spread of disease.
The Problem
In 2013, the CDC classified antibiotic-resistant N. gonorrhoeae as an Urgent Threat9; this organism was added to the next list in 2019 as well.7 This was due to the continued increase in antibiotic resistance observed with N. gonorrhoeae, as total infections and antibiotic resistant cases rose dramatically over the preceding decade. In the last decade or so, the options available to clinicians to treat gonorrheal infections have become more and more limited, because of the worldwide spread of resistance to all available antimicrobial agents, namely penicillins, narrow spectrum cephalosporins, tetracyclines, macrolides, and fluoroquinolones.10 Currently, the US has only a single treatment option that is recommended by the CDC, ceftriaxone. Resistance to this agent has been reported as well but has yet to become widespread (Figure 3; 10). Ceftriaxone and another extended-spectrum cephalosporin (ESC), cefixime, are powerful antibiotics used clinically to treat a variety of infections. Similar to other bacteria, N. gonorrhoeae has several ways to develop resistance to ESCs: by altering the bacterial target of these drugs, by overexpressing a membrane pump that keeps these drugs out of the cells, or by making changes in a membrane protein that blocks the drugs from entering the cells. The ceftriaxone-resistant isolate was identified in Japan in 2011, where there was only limited monitoring of gonococcal antimicrobial resistance, underscoring the urgent need for global surveillance standards.10
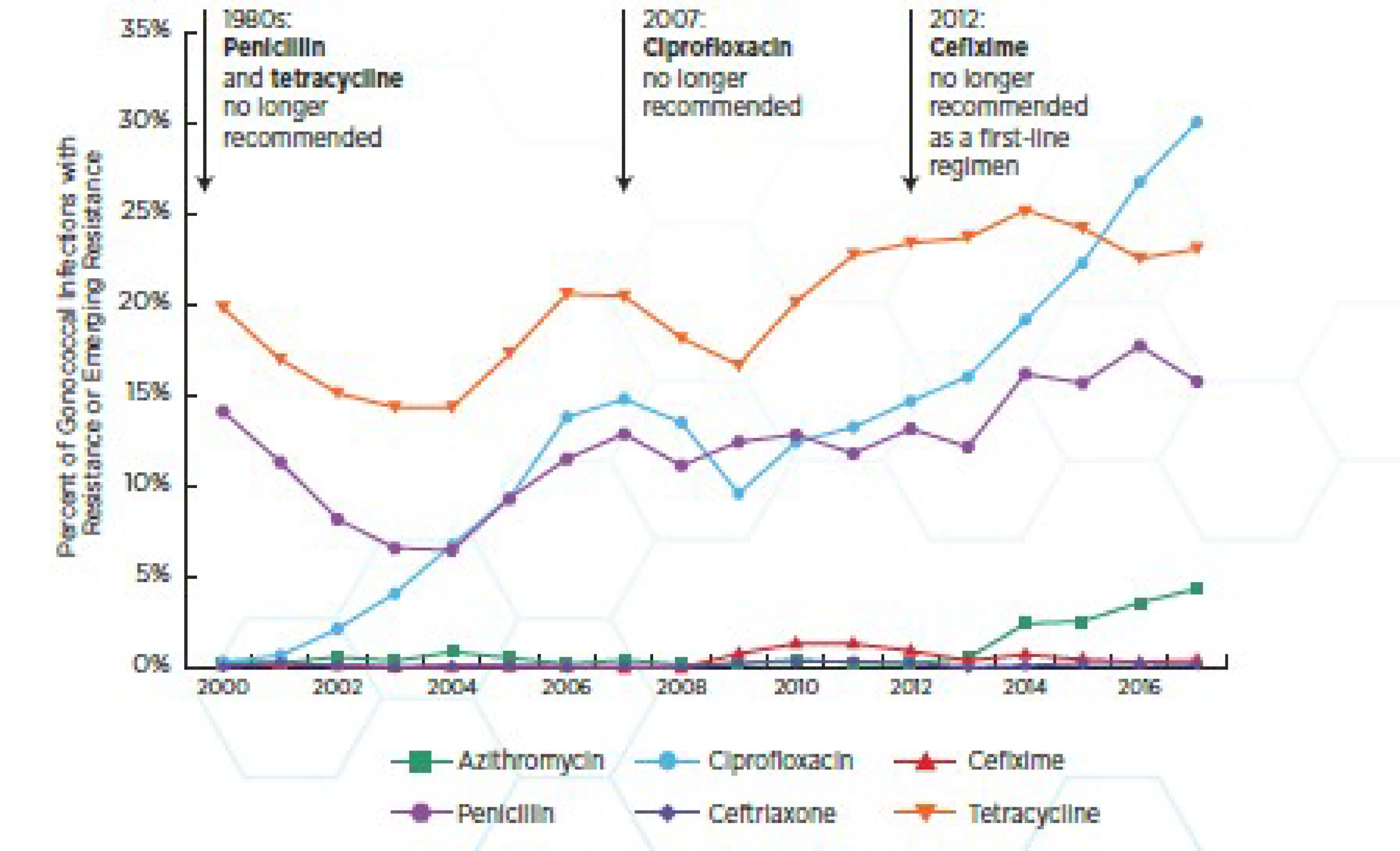
Figure 2: N. gonorrhoeae rapidly develops resistance to antibiotics – ceftriaxone is the last recommended treatment
Source: (7)
Just recently a novel strain of antibiotic-resistant gonorrhea was identified in Massachusetts that was resistant to five classes of antibiotics, the first time such a strain was identified in the US.11 Two apparently unrelated cases were both cured with ceftriaxone, the sole treatment left for gonorrhea.
Contact tracing is underway to determine if other cases resulted from these infections. A lack of known connection between these infections suggests that two strains are circulating independently. Although resistant N. gonorrhoeae isolates have been identified in the UK and Asia-Pacific countries, these are the first reported in the US.11 In another worrisome case, a 50-year-old male patient in Europe returning from a trip to Cambodia was infected with a strain of N. gonorrhoeae that was identified as extensively drug-resistant (XDR), meaning it was only susceptible to one or two antibiotic classes. This isolate resisted a course of ceftriaxone and azithromycin for two weeks; finally, after a course of amoxicillin-clavulanic acid treatment the patient tested negative for N. gonorrhoeae .13
The Response
To help combat the troubling increase in STIs in the last few years, the CDC has put together a network of selected state, county and city health department sentinel sites to follow rates of several STIs and determine the percent compliance within each jurisdiction. The data gathered by this Sexually Transmitted Disease Surveillance Network (SSuN) can also help clinicians and researchers detect emerging antibiotic resistance, how well communities are adhering to CDC treatment guidelines, and rates of EPT for gonorrhea cases.13
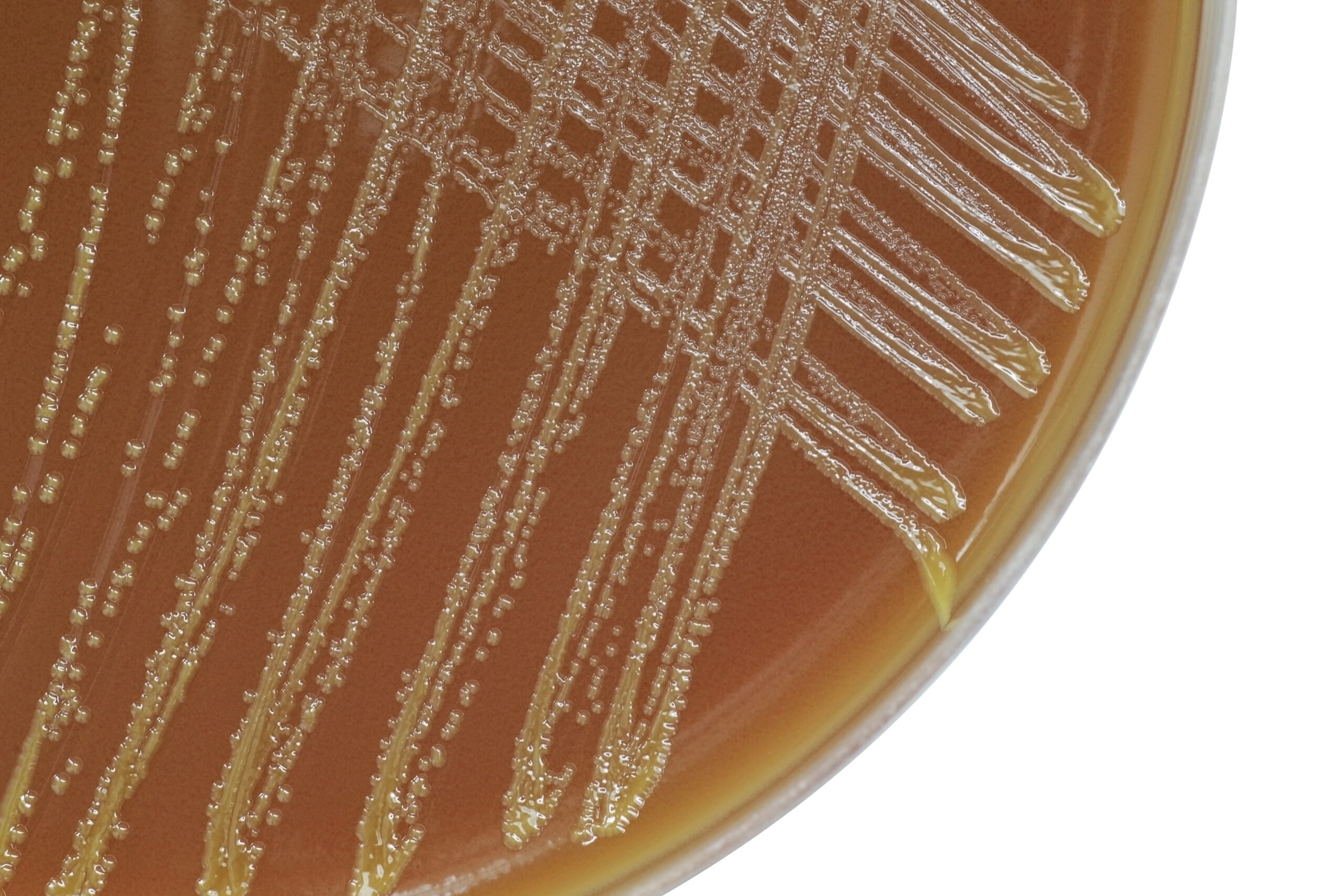
The CDC also runs a program calls GISP, the Gonococcal Isolate Surveillance Project, which was set up in 1986 to follow trends in antibiotic resistance development in N. gonorrhoeae strains in the US to determine the best treatment for these infections based on resistance patterns. Participating STI clinics and their state and local public health authorities, regional laboratories, and the CDC (Figure 4) collaborate in collecting gonococcal isolates monthly from up to the first 25 men with symptomatic gonococcal urethritis seeking care. Isolates are then shipped to regional laboratories for agar dilution susceptibility testing to determine MIC values to penicillin, tetracycline, ceftriaxone, cefixime, ciprofloxacin, azithromycin, and gentamicin. In 2017, a subset of GISP-participating clinical sites expanded their surveillance to include non-urethral isolates (namely, pharyngeal, rectal, and endocervical isolates) – the Enhanced Gonococcal Isolate Surveillance Project (eGISP). The remit of the eGISP program is to help understand whether there are different gonococcal susceptibility patterns between men and women and if these other anatomical sites can select or otherwise foster resistance in this organism. For eGISP, N. gonorrhoeae isolates are collected monthly from up to the first 25 men or women with GC infections of the pharynx or rectum and up to the first 25 women with cervical or vaginal GC infections. GISP monitoring has impacted the CDCs STI Treatment Guidelines as well as the CDCs Antibiotic Resistance Threats Reports in 2013 and 2019.14).
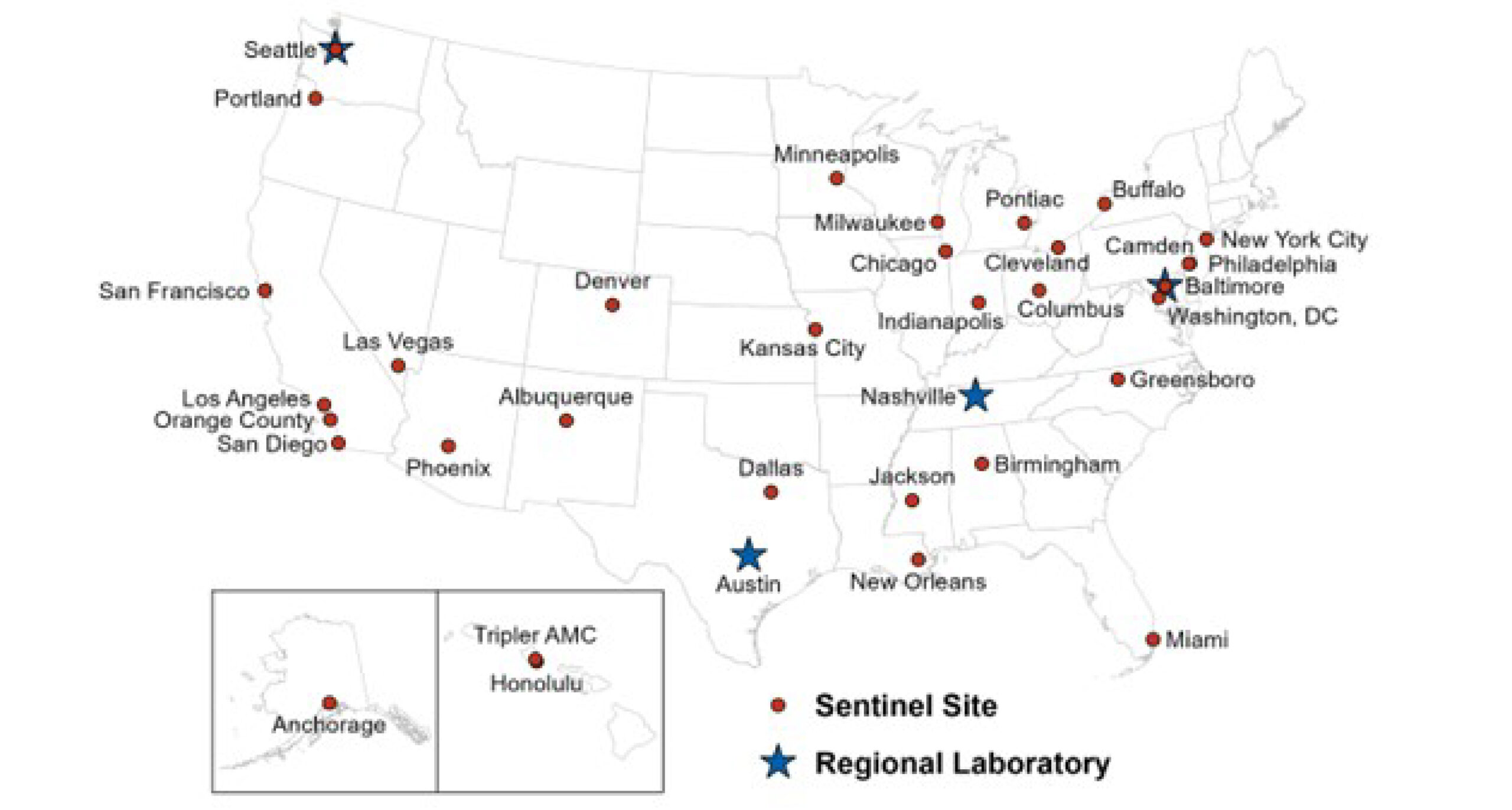
Figure 3: Location of participating sentinel sites and regional laboratories, Gonococcal Isolates Surveillance Project (GISP), 2020 Note: Baltimore and Seattle are both sentinel sites and regional laboratories. Source: (15) slide #31
The WHO Global Gonococcal Antimicrobial Surveillance Program (WHO GASP) was started in 1990 as a global collaborative network to monitor gonococcal antimicrobial resistance across the globe (Figure 5). The WHO also has a joint initiative with Drugs for Neglected Diseases (DND) called the Global Antibiotic Research and Development Partnership (GARDP) that is working to facilitate the development, clinical evaluation and registration of new antibiotics and treatment regimens for gonorrhea. This effort is in tandem with antibiotic stewardship work so that antibiotic resistance to new agents does not rapidly render them useless. Research towards developing a vaccine that would prevent transmission of gonococcus is also ongoing, as WHO officials believe this is likely the only sustainable solution for effectively controlling this infectious disease.
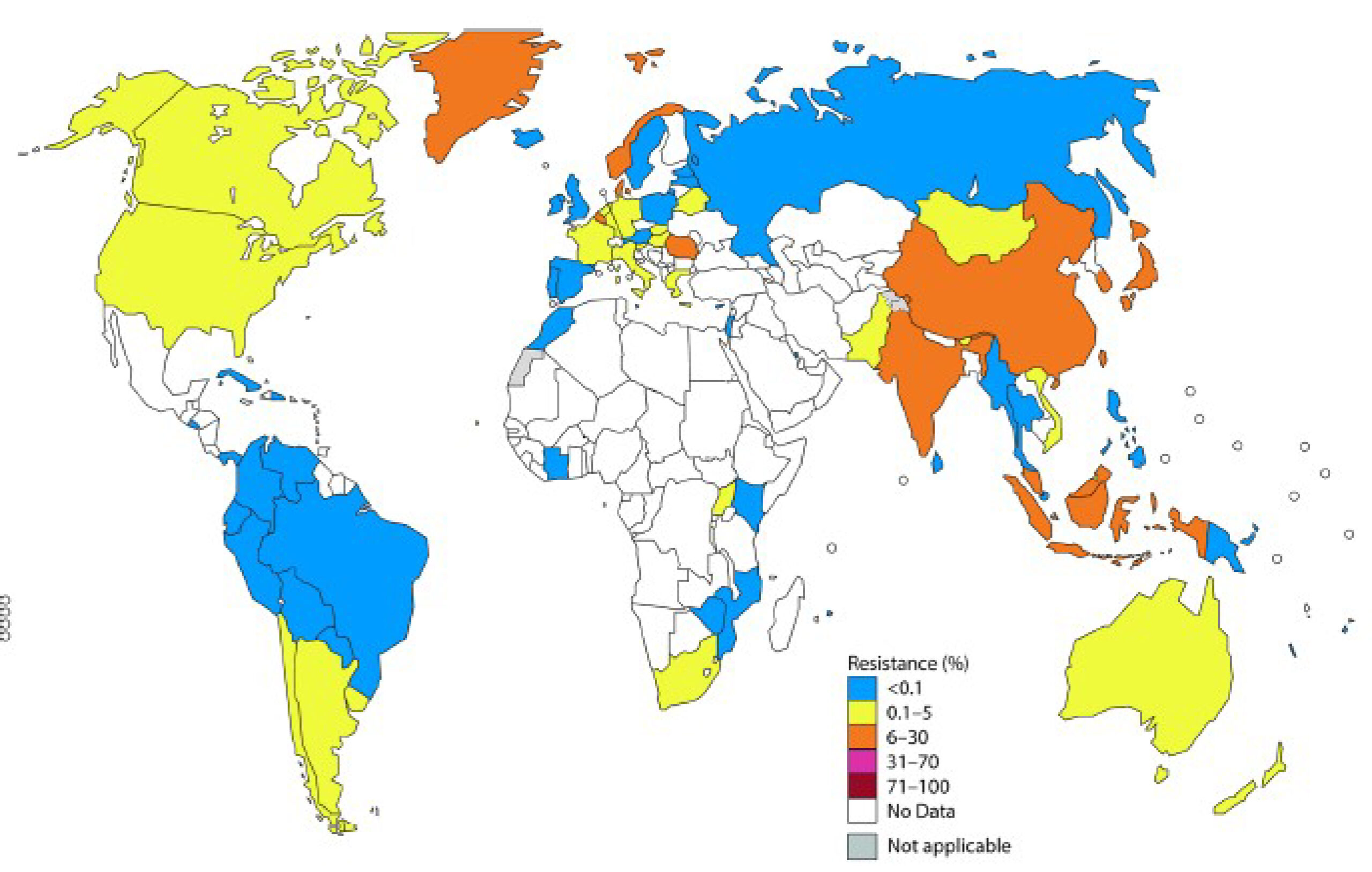
Figure 4: Percentages of N. gonorrheae isolates with resistance to cefixime and/or ceftriaxone per WHO GASP data (2014 for most countries, or 2011 – 2013 for some)
Source: (15)
The Future
New antimicrobials are of course needed, and the urgent hope is for a vaccine; both are subjects of research at several institutions. Other actions including early detection and treatment, contact tracing, antimicrobial stewardship, surveillance of infection, monitoring of antimicrobial resistance and gonorrhea treatment failures and diagnostics.
Resources:
1.) “Incidence, Prevalence, and Cost of Sexually Transmitted Infections in the United States.” CDC. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/2018-STI-incidence-prevalence-factsheet.pdf.
2.) “STI Prevalence, Incidence, and Cost Estimates.” CDC. https://www.cdc.gov/std/statistics/prevalence-incidence-cost-2020.htm.
3.) “Preliminary 2021 STD Surveillance Data.” CDC. https://www.cdc.gov/std/statistics/2021/default.htm.
4.) “Drug-Resistant Gonorrhea: A Public Health Threat.” CDC. https://www.cdc.gov/std/gonorrhea/drug-resistant/public-health-threat/public-health-threat-text-only.htm.
5.) “National Overview of STDs, 2021.” CDC. https://www.cdc.gov/std/statistics/2021/overview.htm#Gonorrhea.
6.) “What’s super about super gonorrhoea? a Q&A with Dr Teodora Wi.” WHO. https://www.who.int/campaigns/world-antimicrobial-awareness-week/2018/features-from-around-the-world/super-gonorrhoea-q-a-with-dr.-teodora-wi.
7.) CDC 2019 AR Threats: 2019 Antibiotic Resistance Threats Report. CDC. https://www.cdc.gov/drugresistance/biggest-threats.html.
8.) “Expedited Partner Therapy.” CDC. https://www.cdc.gov/std/ept/default.htm.
9.) Antibiotic resistance threats in the United States, 2013. CDC. https://stacks.cdc.gov/view/cdc/20705.
10.) Ohnishi, M., et al. 2011. Is Neisseria gonorrhoeae initiating a future era of untreatable gonorrhea?: Detailed characterization of the first strain with high-level resistance to ceftriaxone. Antimicrob Agents Chemother. 55(7): 3538 – 3545.
11.) “Department of Public Health announces first cases of concerning gonorrhea strain.” Department of Public Health. https://www.mass.gov/news/department-of-public-health-announces-first-cases-of-concerning-gonorrhea-strain.
12.) “What is ‘super gonorrhea’? Researchers identify new case in male patient.” WWLP. https://www.wwlp.com/news/health/what-is-super-gonorrhea-researchers-identify-new-case-in-male-patient/.
13.) Shedding Light on Disease in the US: How STD Prevention Programs Benefit from Strong Data. https://www.cdc.gov/std/dstdp/sti-funding-at-work/success-stories/SSuN-Success-Story_FINAL.pdf.
14.) Gonococcal Isolate Surveillance Project (GISP) Profiles, 2020. CDC. https://www.cdc.gov/std/statistics/gisp-profiles/default.htm.
15.) Wi, T, et al. 2017. Antimicrobial resistance in Neisseria gonorrhoeae: Global surveillance and a call for international collaborative action. PLOS Medicine. 14(7): e1002344.





0 Comments